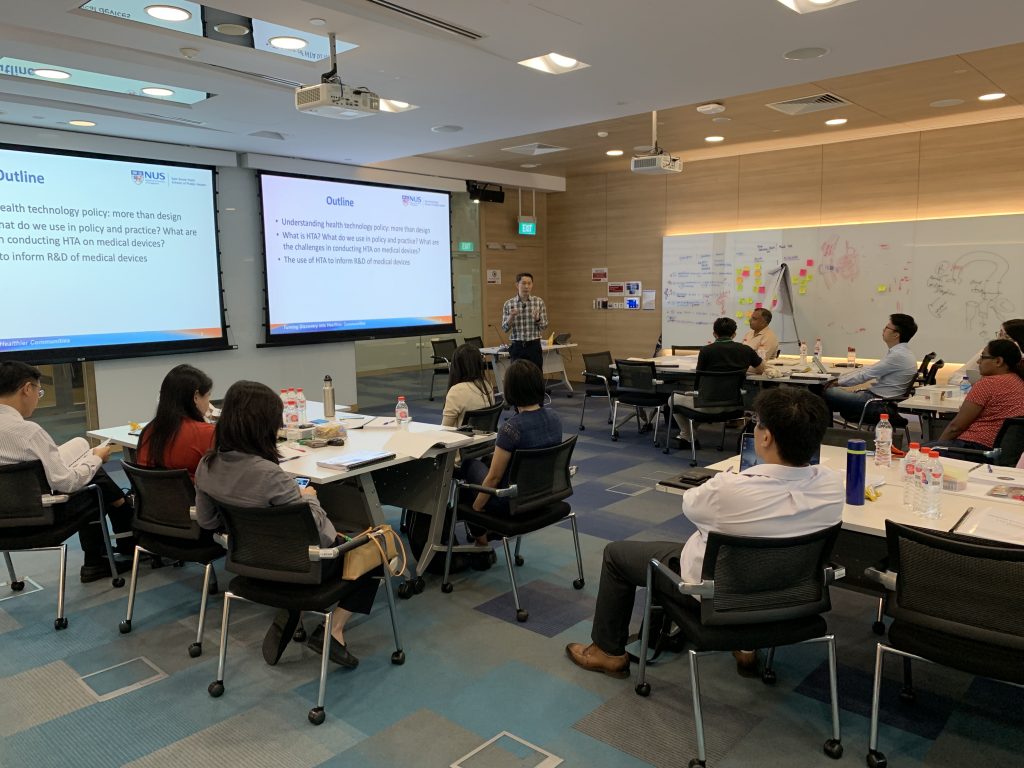
Inaugural HIPER-Singapore Biodesign (SB) HTA Workshop
On 27th May 2019, HIPER and the Agency for Science, Technology and Research (A*STAR)’s Singapore Biodesign co-organised a workshop focusing on early health technology assessment (HTA) processes in the development of medical technologies.
Modelled after the established Biodesign Programme at Stanford University, SB is a capability development initiative that aims to train and nurture the next generation of healthtech innovators for Asia. SB is a dedicated healthtech innovation talent development and knowledge platform essential for health technology innovation startup creation.
The application of early HTA process in the innovation process allows for understanding the magnitude of the problem, identification of outcomes and pricing gaps to be addressed, and demonstration of potential healthcare value for future adoption and reimbursement. The workshop convened 18 participants from the medical device industry, hospitals, and research institutes. Its content and hands-on exercises were structured around playing the roles of (a) policy or decision-makers, (b) HTA researchers, and (c) health technology developers.
Dr Yot Teerawattananon, founder of the Health Intervention and Technology Assessment Program (HITAP) at the Thai Ministry of Health and Visiting Professor at the NUS, led the workshop with the support of five team members. From the perspective of decision-makers, the first priority setting exercise quickly introduced the participants to the bigger picture constraints of resource allocation as well as different approaches for decision-making.
The next segment built incrementally on the first exercise, through a hypothetical case study, where a number of varicose vein reflux treatment strategies were compared. While invasive surgery is the standard of care, new technologies in recent years could potentially offer better value. Applying the HTA methodology, the participants worked through the assessment using a model-based economic evaluation that pitted a hypothetical treatment A against invasive surgery, and worked out the incremental cost-effective ratios (ICERs) using deterministic and probabilistic sensitivity analyses.
Finally, the third section of the workshop was centred around developing a target product profile (TPP) for health technology developers, which aims to inform product development and prevent late stage development failure. The key question posed to the participants was, “Given our knowledge of HTA and the desired properties of similar products, what would be a product profile that could be conducive for future reimbursement decisions?” The participants used threshold analyses in three scenarios that would dominate the market (‘ideal scenario’), produce better value for money compared to current best practice (‘acceptable’), or give value compared to standard of care (‘minimally acceptable’). Again with varicose vein treatment strategies as examples, we examined the three cases using a hypothetical treatment B as the target product.
The post-workshop survey reflected that most participants enjoyed the hands-on learning, but also felt that more time could be allocated to an overview of HTA theory and reimbursement systems in key markets. We look forward to continuing this series and to develop a deeper content and discussion around medical devices in the future.